1601006086 short case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
34 y/m labourer by occupation came with a chief complaints of fever since 10 days
cough since 7 days
sob since 4 days
History of present illness:
Pt was apparently asymptomatic 1 month back then develped SOB which is gr 2 and generalised weakness which is a/w fever (low grade,non continous ,not a/w chills and rigor no diurnal variation )
cough a/w sputum -whitish purulent moderate amounts since 7 days.
SOB gradually progressed from grade 2 to 4 a/w chest tightness and difficulty in breathing no c/o palpitation and syncope attacks
no c/o burning micturition loose stools and constipation
H/o nausea and vomitings
Polyphagia since 2 months
Polyuria since 2months
Past history:
no h/o DM , HTN ,CVA ,CAD, TB ,EPILEPSY .
not significant
personal history
diet:vegeterian
appetite :decreased
bowel and bladder;normal
addictions ;180-360 ml/day since 14 years
16-18 beedis/day
sleep disturbed
family history: no relevant history
General examination:
Patient is conscious coherant and cooperative
ILL built and nourished
No signs of pallor
Icterus
Clubbing
Kolionychia
Lymphadenopathy
Edema
Vital signs :
Blood pressure : 90/60 mm
Pulse rate : 100 per min regular
Respiratory rate - 24 cycles /min
Spo2- 98%
Afebrile
Respiratory system examination:
Decreased breath sounds
Bilateral IAA,ISA
Auscultation:
Bilateral air entry - present
Decreased air entry on left mammary area
And in Infraaxiallary area, infra scapulary area
Wheeze and coarse crepts present
Cardiovascular system examination:
S1 and S2 present
Central nervous system examination:NAD
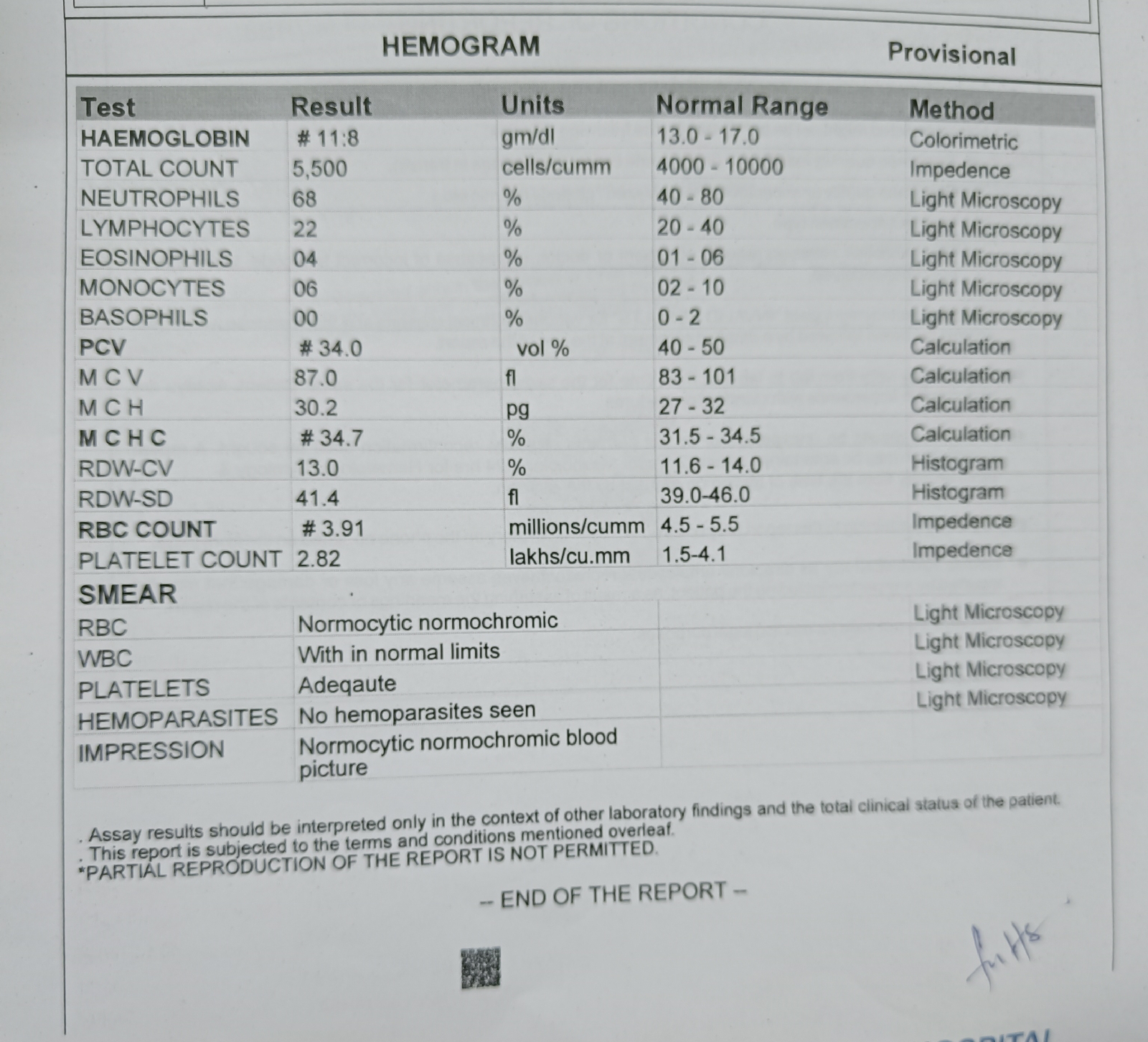
Investigations:
Routine investigations:
Bilateral grade 1 RPD
Chronic pancreatitis
Minimal ascites
DKA with consolidation in left lung
Treatment
IVF -- NS and RL 100ml / hr continuos
Inj pantoo 40mg /IV /OD
Inj augmentin 1.2gm/IV /BD
Tab dolo 650 mg/PO
Syp- ascoryl -p 10 ml/Po /tid
10ml -10ml - 10ml
GRBS charting 2nd hrly
Inj kcl 2 ampoules
In 10 NS
Over 4-5 hours





Comments
Post a Comment