85 year old male
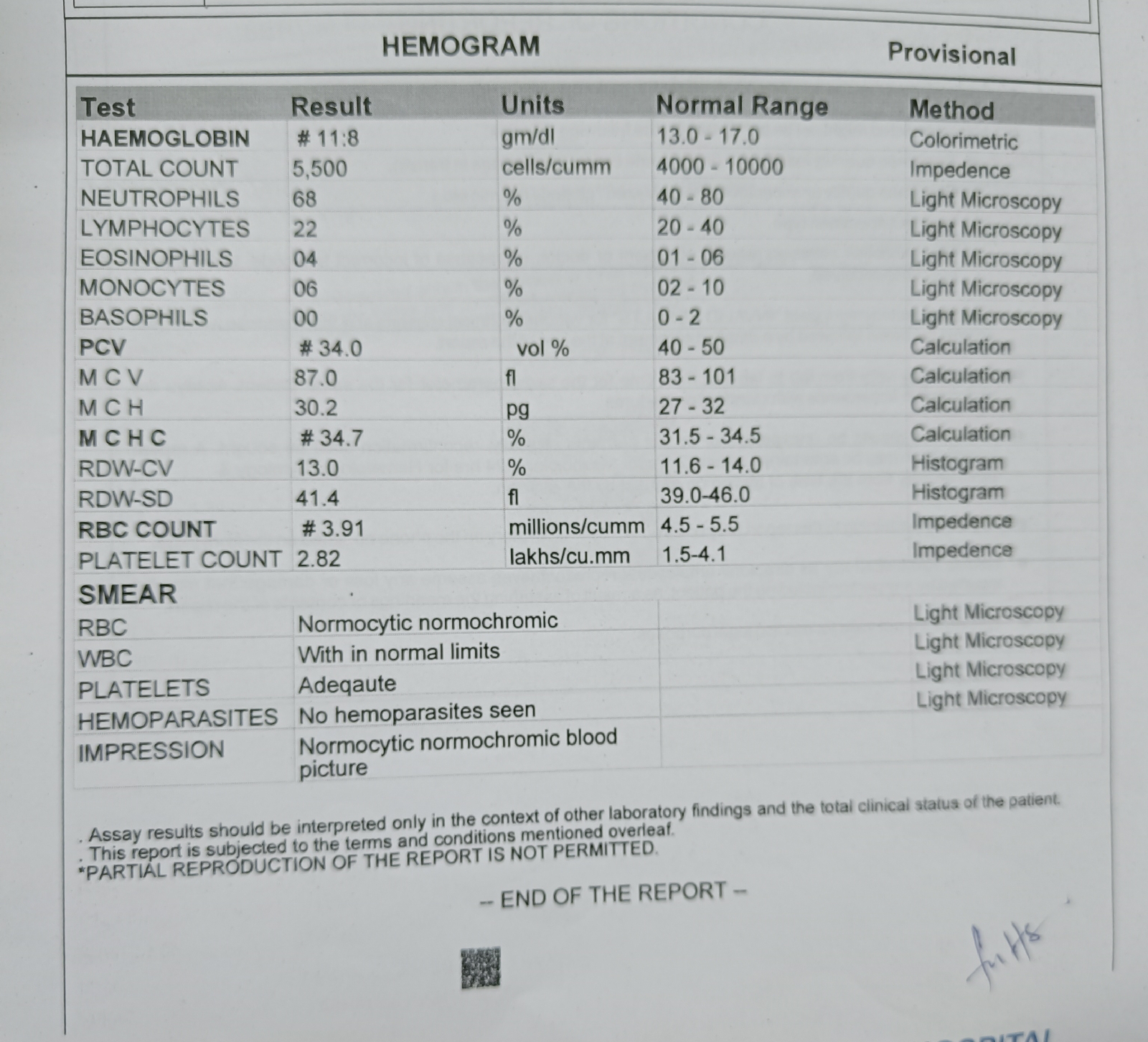
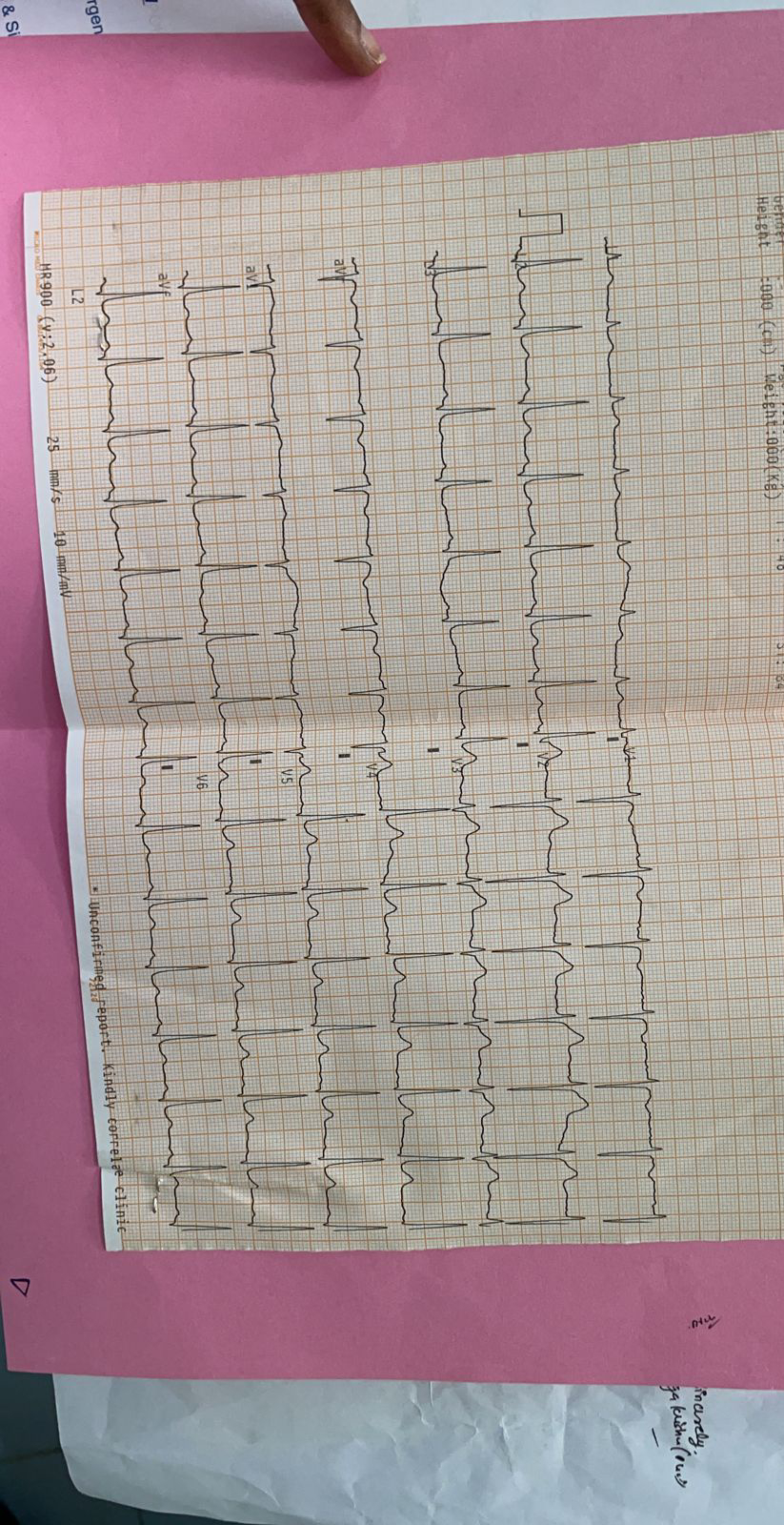
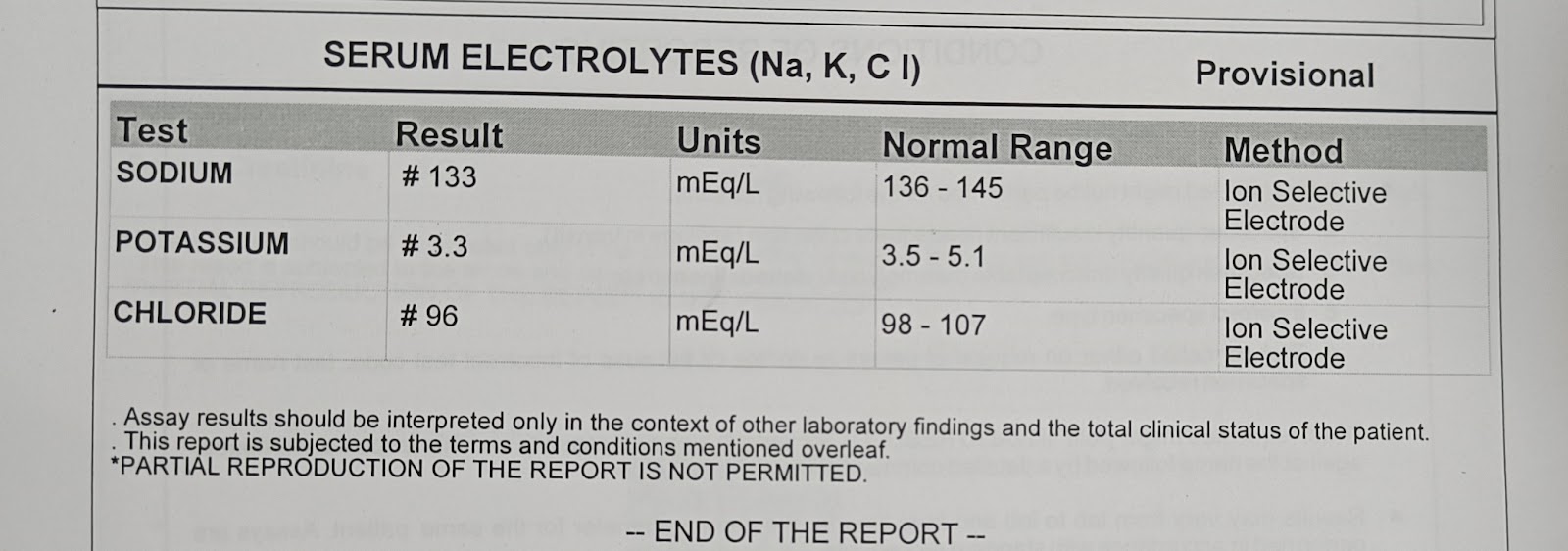
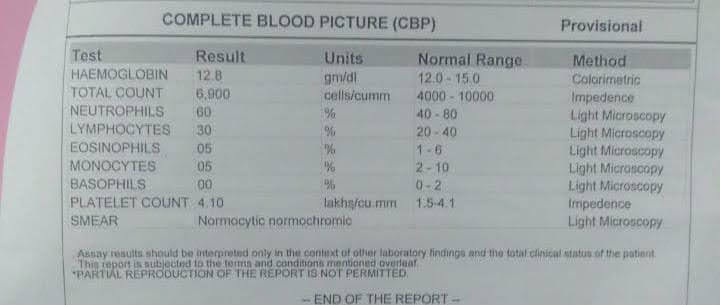
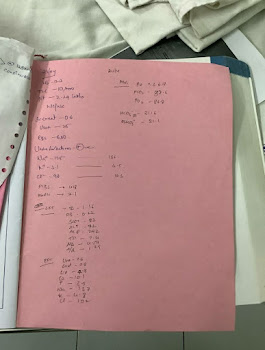
85 year old male came to casualty with chief complaints of weakness of left upperlimb and lowerlimb since 15 days Difficulty in swallowing since 15 days Deviation of mouth towards left side since 15 days No h/o of involuntary micturation No history of involuntary defecation K/C/O HTN and on medication On examination : Patient conscious , coherant , cooperative Past history : Hypertensive and on medication No relevant family and personal history Temperature : afebrile Pulse rate: 100/ min Blood pressure : 140/90 mmhg Respiratory rate : 22 cycles per min SPO2 :99 % at room air GRBS: 198 mg/dl CVS : S1 and S2 heard Respiratory system : NVBS present , BAE present CNS : Conscious speech - normal no signs of meningeal irritation Tone :Increased in left side power: Right. left 4+/5. 4+/5 Reflexes : ...