75 year old male
A 75 year old male patient came to casualty with the complaints of fever and cough since four days
Patient was apparently asymptomatic one week ago. Then , he developed pain abdomen ( generalised ) since 1 week , not associated with vomitings and difficulty in passing stools. He developed fever since 4 days which was high grade associated with chills and cough since 4 days associated with expectoration.
H/O orthopnea present , H/O dribbling of urine .
No H/O pedal edema, PND
K/C/O DM and on OHAs
K/C/O HTN
He is a known alcoholic and last intake was 15 days back.
General examination:
The patient is conscious coherent and cooperative
Moderately built and moderately nourished.
Vitals:
Temp: afebrile, PR 120bpm, RR 22 cpm, BP 110/60mm Hg , GRBS 208 mg%
P/A:
Shape of abdomen: scaphoid
Non tender
Liver and spleen - not palpable
Bowel sounds are present
CVS: S1, S2 +
RS: BAE + , NVBS +
CNS: NFND
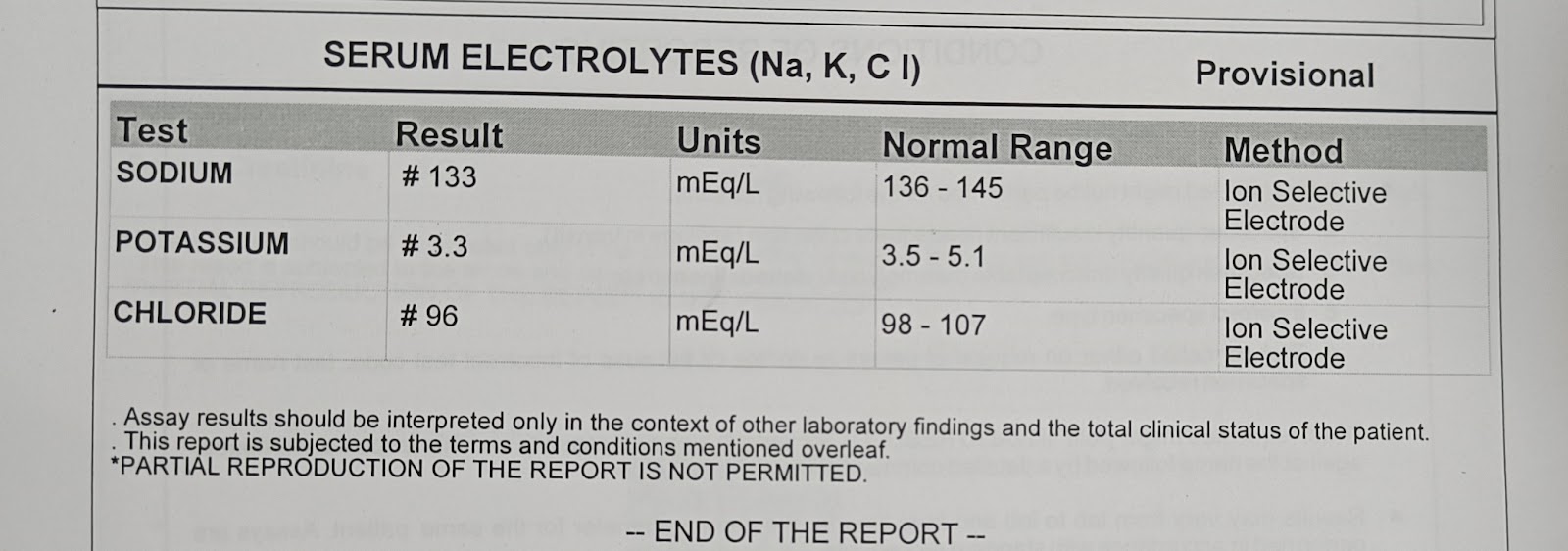
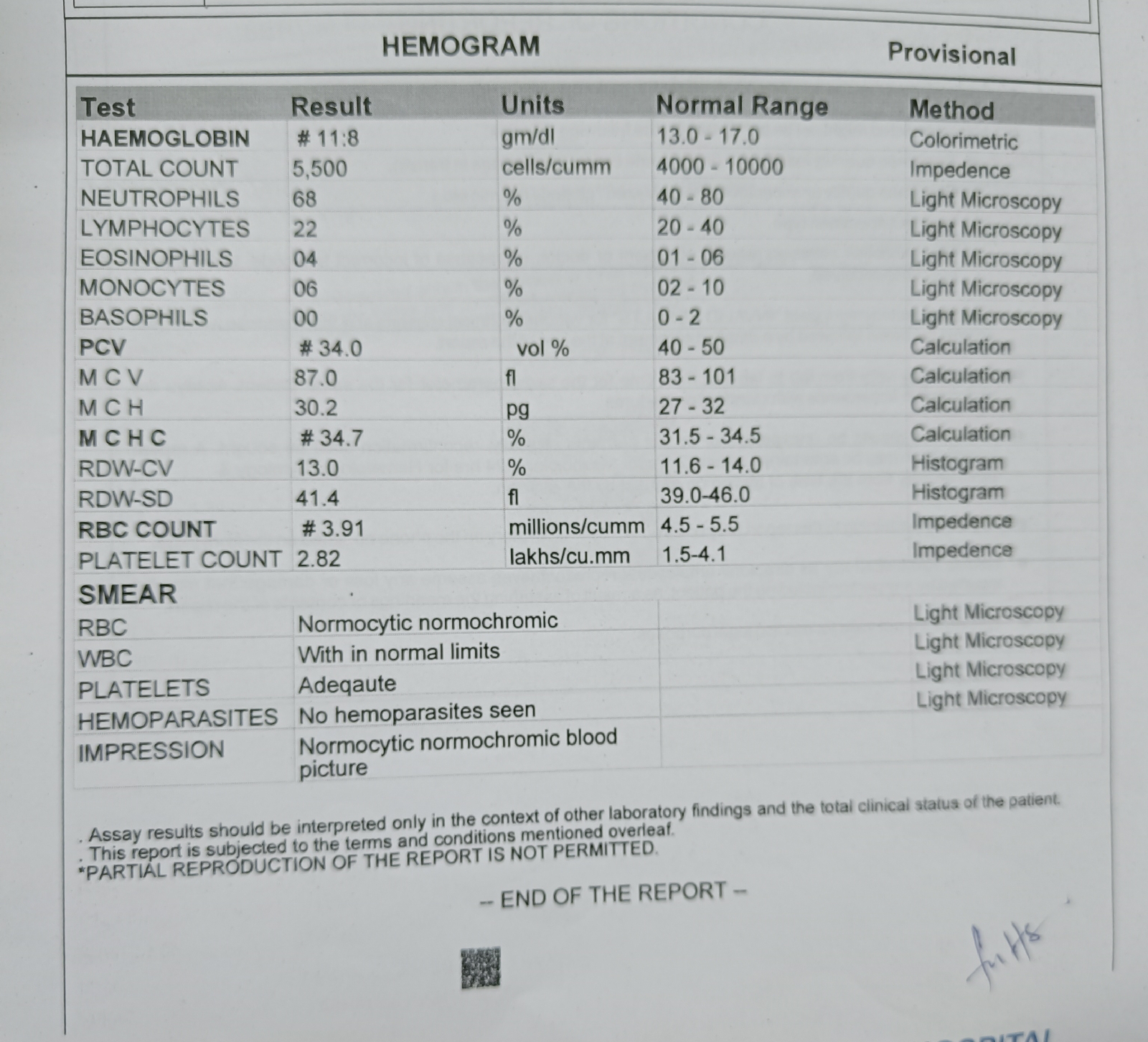
8 /9 /10
ECG on. 7/9/21
ECG on 8 /9/21
Chest x ray :
X ray of both hands ,elbow , ankle joints:
USG abdomen:
1)IVF 0.9 % NS AND RL @ 50 ML / HR
2) ORAL FLUIDS
3) INJ AUGMENTIN 1.2 G/ IV/ BD
4)INJ PAN 40 MG / IV/OD
5) SYP AMBROXOL 10 ML / PO/ TID
6)INJ HAI S/C / TID
7) INJ OPTINEURON 1 AMP IN 100 ML NS /IV/OD
8)TAB PCM 650 MG / PO/TID
9) INJ NEOMOL 1G/IV/SOS
10) NEB WITH BUDECORT , MUCOMIST @ 4 HOURLY
11) SYP CREMAFFIN PLUS 10 ML / PO / H/S
Provisional diagnosis:
Septic shock secondary to pneumonia ( bacterial > viral) ( Right lower lobe consolidation)

























Comments
Post a Comment